Operating Rules
Operating rules support a range of standards to make electronic data transactions more predictable and consistent, regardless of the technology. CAQH CORE is designated by the Secretary of the Department of Health and Human Services (HHS) as the National Operating Rule Authoring Entity for the administrative transactions covered by HIPAA.
Three sets of CAQH CORE Operating Rules are federally mandated under HIPAA. Click the Operating Rules Mandate tab below to access the federally mandated versions of the Eligibility & Benefits, Claim Status and Payment & Remittance Operating Rules. More information is available on the CMS website. CAQH CORE Operating Rule requirements are a floor, not a ceiling, with updated versions of the rules building on the existing requirements. Therefore all federally mandated operating rule requirements are included in the current versions of the CAQH CORE Operating Rules.
Operating Rules
All CAQH CORE Operating Rules are developed through a collaborative, transparent process that ensures balanced representation among participants.
Connectivity
Establishes key connectivity, security and authentication requirements including acknowledgements, error handling, and the CAQH CORE Connectivity “Safe Harbor” creating a national connectivity mechanism that trading partners can be assured will be supported when healthcare information is exchanged. For links to the CORE Connectivity Rules and more detail, please click here.
Eligibility & Benefits
Establishes consistent infrastructure and data content requirements when health plans and providers exchange information regarding a patient’s insurance coverage and benefits. A set of these rules are federally mandated—more information on all CAQH CORE federally mandated rules can be found in the "Operating Rules Mandate" tab on this page.
Current versions CAQH CORE Eligibility & Benefits Operating Rules:
CORE Eligibility & Benefits (270/271) Infrastructure Rule vEB.2.0
CORE Eligibility & Benefits (270/271) Data Content Rule vEB.2.1
Appendix CORE Eligibility & Benefits (270/271) Data Content Rule vEB.2.1
CORE Eligibility & Benefits (270/271) Single Patient Attribution Data Content Rule vEB.1.0
Claim Status
Streamlines the electronic process by which a provider requests the status of a claim and how the health plan responds. A version of this rule is federally mandated.
Current version of the CAQH CORE Claim Status Operating Rule:
Payment and Remittance
Addresses requirements associated with electronic funds transfers (EFT) and electronic remittance advice (ERA), and establishes consistent use of claim adjustment and denial codes. A set of these rules is federally mandated.
Current versions of the CAQH CORE Payment & Remittance Operating Rules:
CORE Payment & Remittance (835) Infrastructure Rule vPR2.0
CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule vPR.1.1
CORE Payment & Remittance (CCD+/835) Reassociation Rule vPR.1.0
CORE Payment & Remittance EFT Enrollment Data Rule vPR.2.0
CORE Required Maximum EFT Enrollment Data Set Companion Document
CORE Payment & Remittance ERA Enrollment Data Rule vPR.2.0
CORE-required Maximum ERA Enrollment Data Set Companion Document
Prior Authorization & Referrals
Standardizes components of the prior authorization process and moves the industry towards full automation.
Current versions of the Prior Authorization & Referrals Operating Rules:
CORE Prior Authorization & Referrals (278) Infrastructure Rule vPA.3.0
CORE Prior Authorization & Referrals (278) Data Content Rule vPA.1.0
CORE Prior Authorization & Referrals Web Portal Rule vPA.1.0
CORE Attachments Prior Authorization Infrastructure Rule vPA.1.0
CORE Attachments Prior Authorization Data Content Rule vPA.1.0
Health Care Claims
Streamlines and standardizes the exchange of information related to the submission, acknowledgement and adjudication of healthcare claims.
Current versions of the CAQH CORE Health Care Claims Operating Rules:
CORE Health Care Claim (837) Infrastructure Rule vHC.2.0
CORE Attachments Health Care Claims Infrastructure Rule vHC.1.0
CORE Attachments Health Care Claims Data Content Rule vHC.1.0
CORE Health Care Claims (837) Data Content Rule vHC.1.0
CORE Claim Acknowledgment Data (277CA) Content Rule vCA.1.0
CORE-required Error Code Combinations for CORE-defined Business Scenarios
Attributed Patient Roster
Attributed patient rosters are used by health plans, providers and employers to share lists of patients attributed to a provider under a value-based contract.
Current versions of the CAQH CORE Attributed Patient Roster Operating Rules:
CORE Attributed Patient Roster (X12 005010X318 834) Data Content Rule vAPR.2.0
CORE Attributed Patient Roster (X12 005010X318 834) Infrastructure Rule vAPR.3.0
Benefit Enrollment
Creates consistent processes and infrastructure requirements for employers, unions, government agencies and other organizations to enroll members in a healthcare benefit plan.
Current version of the CAQH CORE Benefit Enrollment Operating Rule:
CORE Benefit Enrollment and Maintenance (834) Infrastructure Rule vBE.3.0
CORE Benefit Enrollment and Maintenance (834) Data Content Rule vBEM.1.0
Premium Payment
Establishes consistent infrastructure and processes for transmitting information relating to payments.
Current versions of the CAQH CORE Premium Payment Operating Rules:
Rule Development and Voting
All CAQH CORE Operating Rules are developed through a collaborative, transparent process that ensures balanced representation among participants.
| CAQH CORE BODY* | CAQH CORE REQUIREMENTS FOR RULES APPROVAL |
|---|---|
| Level 1: CAQH CORE Subgroups |
Subgroups ensure consensus on initial draft requirements; not addresses in governing procedures. |
| Level 2: CAQH CORE Work Groups |
Work Groups require that a quorum that 60% of participants vote. Simple majority vote (greater than 50%) by this quorum is needed to approve a rule. |
| Level 3: Full CAQH CORE Voting Membership |
Full CORE Voting Membership vote requires that a quorum that 60% of Full CORE Voting Member organizations (i.e., CORE participants that create, transmit, or use transactions) vote on the proposed rule at this stage. With a quorum, a 66.67% approval vote is needed to approve a rule. |
| Level 4: CAQH CORE Board |
The CAQH CORE Board's normal voting procedures apply. If the Board does not approve a proposed operating rule, the Board will issue a memorandum setting forth the reasons it did not approve the proposed operating rule and will ask the work groups to revisit the proposed operating rule. |
*CAQH Board/CAQH does not have veto or voting power over the CAQH CORE Operating Rules.
Updating and Maintaining the CAQH CORE Operating Rules
CAQH CORE Operating Rules set national responsibilities and requirements for timely and accurate use of electronic transactions within the healthcare revenue cycle. To keep up with evolving business needs and new technologies, all operating rules are subject to a cycle of maintenance based on applicability, need and lessons learned.
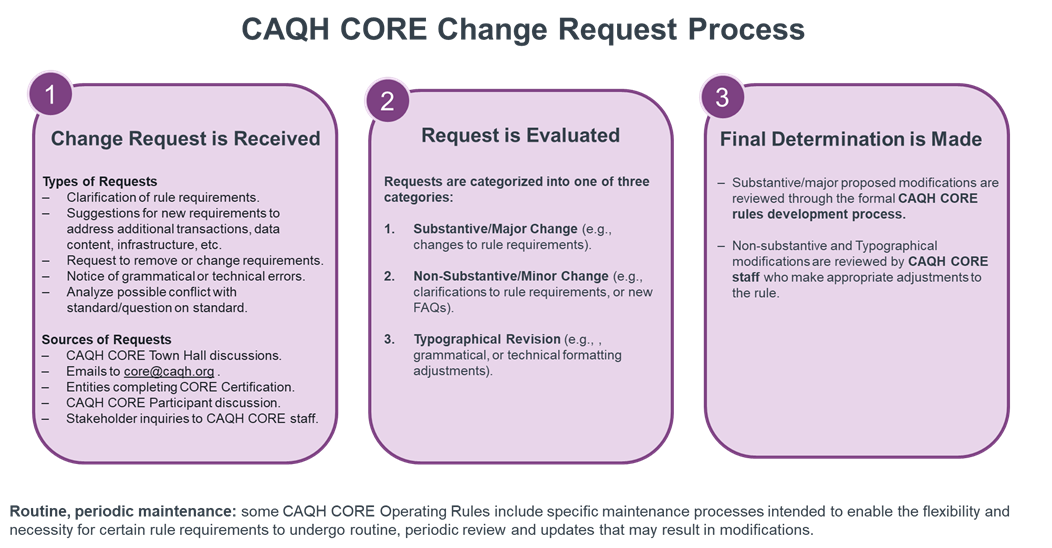
The CAQH CORE Operating Rule Maintenance Process addresses three types of updates: Substantive, Non-substantive, and Typographical, as well as routine, periodic maintenance.
Maintenance and updates to the CAQH CORE Operating Rules are triggered by a variety of reasons:
- New or emerging industry needs.
- Updated versions of the X12 Technical Report Type 3 (TR3) Implementation Specifications or other standards supported by an operating rule.
Routine maintenance is included in the rule. Some CAQH CORE Operating Rules include specific maintenance processes that may result in modifications of the rule. Routine maintenance requirements are outlined in the applicable rules, including the CAQH CORE Payment & Remittance Operating Rules and the CAQH CORE Connectivity Rules.
The CAQH CORE processes to update and publish changes to operating rules depends on the nature of the changes: substantive, non-substantive, typographical or routine, periodic maintenance.
- Substantive changes modify operating rule requirements and require implementers to update their systems. Substantive changes require the formal CORE voting process (see "Rule Development" tab above) be followed, which is an open and balanced process to assure a business need exists, work flow changes are suitable and rule requirements are technically feasible.
Requests for substantive changes can be sent to CORE@caqh.organd will be considered by CAQH CORE Participants. If a request identifies an issue that may impede or prevent industry implementation of an operating rule, it will be prioritized and addressed by the appropriate CAQH CORE work group.
- Non-substantive changes do not materially impact implementers that need to comply with the operating rules. Examples of non-substantive changes include adding explanatory text or removing content from operating rules that has been incorporated into a new mandated version of the underlying standard. Non-substantive changes do not require the formal CAQH CORE voting process.
Note: Since CAQH CORE Operating Rules do not repeat the HIPAA-mandated “minimum” requirements in the HIPAA-mandated X12 TR3 Implementation Specifications, in the event that new versions of X12 TR3 Implementation Specifications or other standards are mandated under HIPAA, appropriate revisions to the CAQH CORE Operating Rules are made and a draft available for public input. For example, the CAQH CORE Operating Rules were updated when HIPAA mandates moved from v4010 to v5010 of the X12 standards.
- Typographical revisions have no impact on implementers as they do not change operating rule requirements and involve corrections to grammatical and technical errors found in operating rules. Examples of typographical errors include misspelling of words, a misprint, technical formatting adjustments or adjustment in punctuation. Typographic revisions do not require the formal CAQH CORE voting process.
- Periodic, routine maintenance does not change underlying operating rule requirements, but upgrades content requirements based on industry needs and lessons learned. This type of maintenance – which focuses on a specific rule requirement - requires a formal and transparent process to collect multi-stakeholder input. This process is used for the CAQH CORE Code Combinations Maintenance Process and the EFT & ERA Enrollment Data Sets Maintenance Process.
The CAQH CORE Operating Rule Change Process is depicted below.
When substantial updates that modify rule requirements are made to an operating rule, its major version number is updated. If non-substantive updates are made to an operating rule, such a wording changes or providing additional clarification, the minor version is updated. Typographical revisions will not result in a version number update.
As changes are made to an operating rule, CAQH CORE will issue an erratum within the Revision History section to describe the updates and versioning impact.
Routine, periodic maintenance to operating rules may result in a substantive, non-substantive or typographical revisions
CAQH CORE Version Identification Scheme
Key to effectively managing and maintaining these various potential CAQH CORE Operating Rule updates is the careful and precise assignment of version identifiers to the rules and any of their companion documents. This version identification scheme is shown below.
| OR.1.0 | No impact to versioning | ||
|---|---|---|---|
| Primary rule version designating CAQH CORE rule set (requires all CAQH CORE Vote) | Substantive revision to the rule (modifies a rule requirement and requires CAQH CORE Participant Approval) | Non-substantive revision to the rule (wording changes for meaning clarification, remove ambiguity – no change to a rule requirement) | Typographical revision to the rule that corrects grammatical and/or technical formatting - no change to a rule requirement; no impact no implementation; no versioning change. |
Operating Rules or Enhancement to Existing
Operating Rules
CAQH CORE welcomes industry ideas and input on potential new and updated operating rules. New operating rules could address data content suggestions for HIPAA-mandated transactions, as well as transactions not mandated under HIPAA. The CAQH CORE Board relies on key feedback mechanisms including CAQH CORE surveys, work group feedback, the maintenance processes and industry feedback received at core@caqh.org to prioritize rule development and maintenance efforts.
CAQH CORE is committed to conducting substantive, non-substantive, typographical, and routine maintenance on existing rules and developing new rules as appropriate. All rule development and maintenance is conducted by CAQH CORE Participating Organizations and is performed in accordance with the CAQH CORE Operating Rules Development Process in alignment with the CAQH CORE mission and vision.
HIPAA-mandated Healthcare Operating Rules
Section 1104 of the Patient Protection and Affordable Care Act (ACA) requires the Secretary of the Department of Health and Human Services (HHS) to adopt and regularly update standards, implementation specifications and operating rules for the electronic exchange and use of health information for the purposes of financial and administrative transactions under HIPAA. This section applies to HIPAA covered entities and business associates engaging in HIPAA standard transactions on behalf of covered entities.
The ACA defines operating rules as “the necessary business rules and guidelines for the electronic exchange of information that are not defined by a standard or its implementation specifications."
CAQH CORE is designated by the Secretary of HHS as the Operating Rule Authoring Entity for the HIPAA-mandated administrative transactions. CAQH CORE Operating Rules addressing eligibility & benefits, claim status and payment & remittance are federally mandated.
View the CMS website for more detail on the Administrative Simplification provisions of the ACA.
Learn how CMS enforces Administrative Simplification requirements by watching this video.
Accessing the HIPAA-mandated Versions of the CAQH CORE Operating Rules
In 2020, CAQH CORE updated its phase-based operating rule structure to align with current stakeholder operations. The CAQH CORE Operating Rules are now organized by the business processes they support which enhances flexibility to update requirements, enables more rapid and targeted rule development and eliminates the potential for an infinite number of future operating rule phases.
While the CAQH CORE Eligibility & Benefits, Claim Status and Payment & Remittance Operating Rule versions have been updated to meet current and emerging business needs, all of the requirements included in the HIPAA-mandated rule versions remain in the current versions.
Below, are links to the federally mandated versions of the operating rules and the most recent version.
| Former Operating Rule Name | Former Version | Current Operating Rule Name | Current Version |
|---|---|---|---|
| CAQH CORE ELIGIBILITY & BENEFITS (EB) OPERATING RULE SET | |||
| Phase I CORE 152: Eligibility and Benefit Real Time Companion Guide Rule | v1.1.0 | CAQH CORE Eligibility & Benefits (270/271) Infrastructure Rule All eligibility infrastructure requirements combined into a single infrastructure rule. |
vEB.2.0 |
| Phase I CORE 155: Eligibility and Benefits Batch Response Time Rule | V.1.1.0 | ||
| Phase I CORE 156: Eligibility and Benefits Real Time Response Time Rule | V.1.1.0 | ||
| Phase I CORE 157: Eligibility and Benefits System Availability Rule | V.1.1.0 | ||
| Phase I CORE 154: Eligibility and Benefits 270/271 Data Content Rule | v1.1.0 | CAQH CORE Eligibility & Benefits (270/271) Data Content Rule All eligibility data content requirements combined into a single data content rule. |
vEB.1.0 |
| Phase II CAQH CORE 260: Eligibility & Benefits Data Content (270/271) Rule | V.2.1.0 | ||
| Phase II CAQH CORE 258: Eligibility and Benefits 270/271 Normalizing Patient Last Name Rule | V.2.1.0 | ||
| Phase II CAQH CORE 259: Eligibility and Benefits 270/271 AAA Error Code Reporting Rule | V.2.1.0 | ||
| Phase I CORE 153: Eligibility and Benefits Connectivity Rule | V.1.1.0 | CAQH CORE Connectivity Rule | vC1.1.0 |
| Phase II CAQH CORE 270: Connectivity Rule | V.2.2.0 | CAQH CORE Connectivity Rule | vC2.2.0 |
| CAQH CORE CLAIM STATUS (CS) OPERATING RULE SET | |||
| Phase II CAQH CORE 250: Claim Status Rule | V.2.1.0 | CAQH CORE Claim Status (276/277) Infrastructure Rule | vCS.1.0 |
| Phase II CAQH CORE 270: Connectivity Rule | V.2.2.0 | CAQH CORE Claim Status (276/277) Infrastructure Rule | vC2.2.0 |
| CAQH CORE PAYMENT & REMITTANCE (PR) OPERATING RULE SET | |||
| Phase III CORE 350 Health Care Claim Payment/Advice (835) Infrastructure Rule | V.3.0.0 | CAQH CORE Payment & Remittance (835) Infrastructure Rule | vPR.1.0 |
| Phase III CORE 360 Uniform Use of Claim Adjustment Reason Codes and Remittance Advice Remark Codes (835) Rule | V.3.0.0 | CAQH CORE Payment & Remittance (835) Uniform Use of CARCs and RARCs Rule | vPR.1.0 |
| Phase III CORE 370 EFT & ERA Reassociation (CCD+/835) Rule | V.3.0.0 | CAQH CORE Payment & Remittance (CCD+/835) Reassociation Rule | vPR.1.0 |
| Phase III CORE 380 EFT Enrollment Data Rule | V.3.0.0 | CAQH CORE Payment & Remittance EFT Enrollment Data Rule | vPR.1.0 |
| Phase III CORE 382 ERA Enrollment Data Rule | V.3.0.0 | CAQH CORE Payment & Remittance ERA Enrollment Data Rule | vPR.1.0 |
| Phase II CAQH CORE 270: Connectivity Rule | V.3.0.0 | CAQH CORE Connectivity Rule | vC2.2.0 |
| CAQH CORE MASTER COMPANION GUIDE | |||
| CAQH CORE Master Companion Guide Template | V5010 | CAQH CORE Master Companion Guide Template | version agnostic |
Keeping Up with the CORE Code Combinations
Current Version of the CORE Code Combinations: February 2026 v3.10.0
If you have been tasked with implementing the CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule, part of the Affordable Care Act (ACA)-mandated Payment & Remittance Operating Rules, you will find all the necessary tools and information here to comply with this operating rule.
These resources are provided free of charge by CAQH CORE, author of the operating rules, and are intended to help organizations comply with the law.
Background
The CAQH CORE Payment & Remittance Operating Rules, among other things, simplify the language used to communicate about claim payment and remittance information. The CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule brings uniformity to the use of Claim Adjustment Reason Codes (CARCs), Remittance Advice Remark Codes (RARCs), and Claim Adjustment Group Codes (CAGCs) by identifying a limited set of CARC/RARC/CAGC combinations to be used in defined universal business scenarios. These codes are used in combination to convey details about a claim adjustment or denial in the X12 v5010 835.
Together, the business scenarios and code combinations make up the CORE-required Code Combinations for CORE-defined Business Scenarios (CORE Code Combinations), a companion document to the CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule.
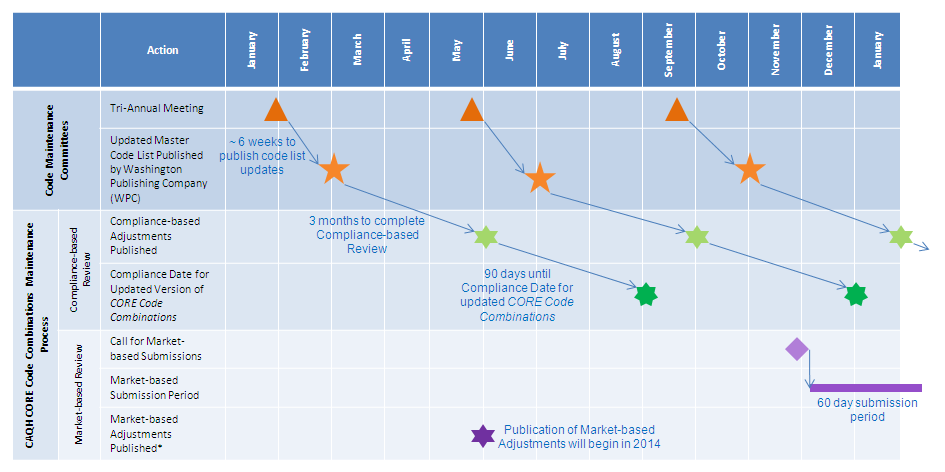
The published CARC and RARC lists and, in turn, the CORE Code Combinations are updated three times per year.
The current version of CORE Code Combinations for use with the CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule is the CORE Code Combinations February 2026 v3.10.0
As the table illustrates, this version aligns with CARC and RARC list updates published November 1, 2025.
High-level Summary of Adjustments in Version 3.10.0 of the CORE Code Combinations
Version 3.10.0 of the CORE Code Combinations includes updates based on a Compliance-based review as part of the CAQH CORE Code Combinations Maintenance Process.
The table below summarizes the Market-based Adjustments approved by the CAQH CORE Code Combinations Task Group for inclusion in the current version of the CORE Code Combinations by CORE-defined Business Scenario.
| Type of Adjustment | CORE-defined Business Scenario #1 | CORE-defined Business Scenario #2 | CORE-defined Business Scenario #3 | CORE-defined Business Scenario #4 |
|---|---|---|---|---|
|
November 2025 Compliance and Market-based Review |
N/A |
Addition of RARC M74 to existing CARC 4; addition of RARCs M66, N206, N684 to existing CARC 16; addition of RARC M86 to existing CARC 18; addition of RARCs M20 and N386 to existing CARC 189 |
Addition of RARC N428 to existing CARC 5; addition of RARC M25 to existing CARC 11; addition of RARC MA04 to existing CARC 19; addition of RARC M7 to existing CARC 35; addition of RARC N429 to existing CARC 50; addition of RARC M25 to existing CARCs 54 and 56; addition of RARCs M2, M77, and N428 to existing CARC 58; addition of RARC M2 to existing CARC 60; addition of RARCs M51, M64, N67, and N301 to existing CARC 96; addition of RARC M25 to existing CARC 108; addition of RARC N115 to existing CARC 109; addition of RARC M40 to existing CARC 111; addition of RARC N362 to existing CARC 149; addition of RARCs N180 and N205 to existing CARC 150; addition of RARCs M52, M83, M90, N20, and N180 to existing CARC 151; addition of RARCs M64 and N372 to existing CARC 167; addition of RARCs N115 and N121 to existing CARC 170; addition of RARC N95 to existing CARC 171; addition of RARC N535 to existing CARC 172; addition of RARC N30 to existing CARC 177; addition of RARCs N61, N67, and N83 to existing CARC 239; addition of RARCs N56 and N819 to existing CARC 272; addition of RARC MA63 to CARC B9; Addition of RARC N115 to existing CARC B13; addition of RARCs N115, MA133, N67, and N130 to existing CARC B15; and addition of RARCs M2, MA12, and N115 to existing CARC B20. |
Addition of RARC M14 to existing CARC 97. |
Summary of Compliance-based Adjustments in Version 3.10.0 of the CORE Code Combinations
| November 2025 Adjustments to Published Code Lists | CORE Code Combinations v3.10.0 February 2026 Compliance-based Adjustments |
|---|---|
|
Deactivations |
N/A |
|
Modifications |
N/A |
|
Additions |
N/A |
Overview of Market-based Review Process and Scope
CAQH CORE facilitates a public 60-day period during which industry entities can submit potential Market-based Adjustments to code combinations in the existing CORE-defined business scenarios. Industry entities can submit three categories of potential code combination adjustments:
- Addition of new CORE Code Combinations.
- Removal of existing CORE Code Combinations.
- Relocation of an existing CORE Code Combination from an existing CORE-defined Business Scenario to another existing CORE-defined Business Scenario.
Summary of Market-based Adjustments in the February 2026 Version of the CORE Code Combinations
| Type of Adjustment | CORE-defined Business Scenario #1 | CORE-defined Business Scenario #2 | CORE-defined Business Scenario #3 | CORE-defined Business Scenario #4 |
|---|---|---|---|---|
| Additions |
N/A |
|
|
|
| Removals |
N/A |
N/A |
N/A |
N/A |
The CORE Code Combinations are updated at scheduled intervals to align with updates to the published CARC and RARC lists, which are maintained by CARC/RARC Code Committees external to CAQH CORE. The following table illustrates the timeline.
| Projected Dates of CARC & RARC List Updates | Scheduled Publication Date of CORE Code Combinations (approximately 3 months after list updates) |
Mandated Compliance Date for CORE Code Combinations (90 days after date of publication) |
|---|---|---|
| ~November 1 | February 1 | May 1 |
| ~March 1 | June 1 | September 1 |
| ~July 1 | October 1 | January 1 |
Beginning January 1, 2014, HIPAA-covered entities have 90 days to comply with published updates to the CORE Code Combinations.
Exception: In some instances, the effective date for code modifications and deactivations approved by the code maintenance committees is more than six months after publication of the updated code list. To accommodate code modifications or deactivations that go into effect after the compliance date for the new version of the CORE-required Code Combinations for CORE-defined Business Scenarios (e.g. adjustments with effective dates greater than six months from the code list publication date), CAQH CORE has incorporated the following exceptions to the 90 day compliance timeframe:
- Any deactivated CORE-required CARCs and RARCs may continue to be used until the effective deactivation/stop date as published by the respective code maintenance committee.
- Any modified CORE-required CARCs and RARCs may continue to be used with their previous description until the effective date of the code description modification as published by the respective code maintenance committee.
After the effective date, the unmodified or deactivated code can only continue to be used in “derivative business transactions”. Derivative business transactions are business messages where the CARC or RARC is being reported from an original business message that was initiated prior to the code adjustment effective date.
NOTE: The 04/19/13 CMS Notice to the Industry states that because the Maintenance Process was adopted in the IFC, covered entities should understand that revised and updated versions of the CORE Code Combinations are part of the regulation (applies to both Compliance and Market-based Adjustments to current CORE-defined Business Scenarios); covered entities are responsible for complying with the latest version.
The CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule requirements and the impact of updated versions of the CORE Code Combinations vary depending on an entity’s stakeholder type.
NOTE: ACA Section 1104 mandates that all HIPAA covered entities comply with the Payment & Remittance Operating Rules; however non-HIPAA covered entities play a crucial role in enabling their provider and health plan clients to realize the benefits of industry adoption and often act as Business Associates on behalf of a HIPAA covered entity.
| Creators of the X12 v5010 835 | Receivers of the X12 v5010 835 | |
|---|---|---|
| Applicable Stakeholder Types | Creators of the X12 v5010 835
Any organization with systems that creates the X12 v5010 835, which may include:
|
Receivers of the X12 v5010 835
Any organization with systems that receive the X12 v5010 835 and extracts data for manual processing, which may include:
|
|
What requirements apply to my organization?
(Please refer to CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule for a full list of applicable rule requirements) |
Creators of the X12 v5010 835
Systems creating the X12 v5010 835 must have the ability to:
|
Receivers of the X12 v5010 835
When receiving a v5010 X12 835, a product extracting the data from the X12 v5010 835 for manual processing must make available to the end user:
|
| What does my organization need to do when an updated version of the CORE Code Combinations is published? | Creators of the X12 v5010 835
Organizations with systems that create the X12 v5010 835 should:
|
Receivers of the X12 v5010 835
Organizations with products that receive the X12 v5010 835 and extract data for manual processing should:
Providers should:
|
The CARC and RARC lists are authored and maintained by CARC/RARC Code Committees designated by the Secretary of Health and Human Services. Addition, modification, or removal of codes must be addressed by the appropriate committee, either the Claim Adjustment Status Code Maintenance Committee or Remittance Advice Remark Code Committee; this is out of scope for CAQH CORE. The CARC/RARC Code Committees meet and publish updates on the Washington Publishing Company’s website three times per year. The CAGCs are part of the X12 835 standard and are thus maintained by ASC X12.
| CARCs (Claim Adjustment Status Code Maintenance Committee) |
RARCs (Remittance Advice Remark Code Committee) |
CAGCs (ASC X12) |
|---|---|---|
|
|
|
The CORE Code Combinations are maintained by the CAQH CORE Code Combinations Task Group.
The CAQH CORE Code Combinations Task Group conducts two types of reviews and adjustments of the CORE Code Combinations as part of its ongoing CAQH CORE Code Combinations Maintenance Process required by the CAQH CORE Payment & Remittance Uniform Use of CARCs and RARCs (835) Rule:
Compliance-based Reviews: Occur three times per year and consider only additions, deactivations, or modifications to the current published CARC and RARC lists by the code committees since the last update to the CORE Code Combinations
Market-based Reviews: Occur once every two years and address ongoing and evolving industry business needs. A Market-based Review considers industry submissions addressing:
Adjustments to the existing CORE Code Combinations for existing CORE-defined Business Scenarios (additions, removals, etc.) based on real-world usage data and/or a strong business case
Addition of new CORE-defined Business Scenarios and associated CORE-required Code Combinations based on real-world usage data and a strong business case
CAQH CORE has also established a Code Combinations Emergency Update Process.
The timeline below lays out the general timeframes for the CARC/RARC Code Committees and the CAQH CORE Code Combinations Maintenance Process.
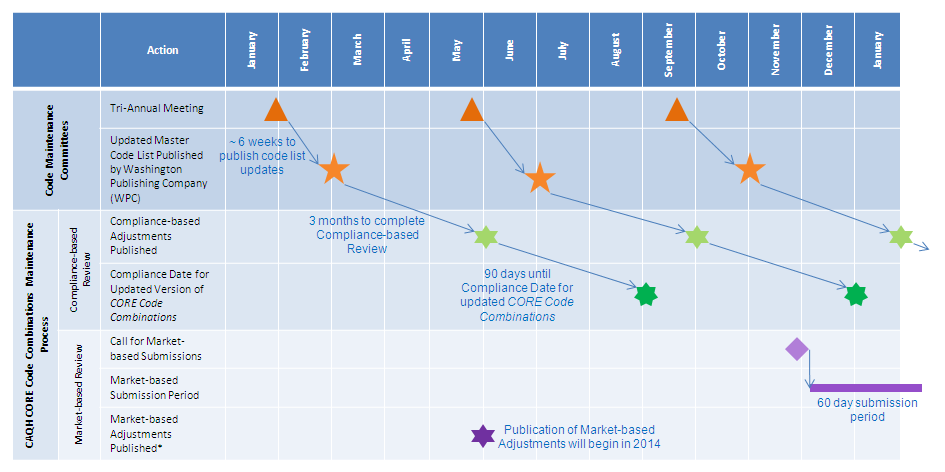
*Goal is to publish the Market Adjustments with Compliance-based Adjustments to ensure only 3 annual updates to the CORE Code Combinations.
To learn more about the CORE Code Combinations Maintenance Process, see the FAQs for CAQH CORE Use of CARCs & RARCs Rule.
The CAQH Committee on Operating Rules for Information Exchange (CORE) Market-based Review will re-open in 2026. Questions about the process and how to become involved can be sent to CORE@caqh.org
INTERESTED IN JOINING CORE OR THE CORE CODE COMBINATIONS TASK GROUP?
- You can learn more about CORE by clicking here.
- Please email us at CORE@caqh.org for more information on how to join us for this important work.
If you need additional assistance in navigating the Market-based Adjustments Form or have any questions regarding the 2024 MBR, feel free to respond directly to this email or contact Michael Phillips, Director, Advisory & Insights, at mphillips@caqh.org.
Entities are encouraged to join CAQH CORE as a Participating Organization to:
- Contribute to the evolution of CAQH CORE Use of CARCs & RARCs Rule and the CORE Code Combinations via the CAQH CORE Code Combinations Task Group.
- Have a voice in the development of operating rules.
- Be part of a solution that is taking cost and complexity out of the healthcare system.
CAQH CORE welcomes Participating Organizations representing a range of stakeholder groups.
Entities can also contribute a number of other ways, for example:
- Submission of Market-based Adjustments to the CORE Code Combinations.
- Work directly with CMS, standard setting bodies like ASC X12, and the various industry code committees to advance industry knowledge.
- Respond to public surveys or submit requests to CORE@caqh.org.
Trading Partner Collaboration: Conformance Testing and Voluntary CORE Certification
- Conformance testing with your trading partners is a critical aspect to making your operating rules implementation a success.
- HIPAA covered entities can quickly communicate their organization’s readiness to testing their conformance with trading partners by adding their company information to the CORE Partner Testing page of the CAQH website.
- Entities should consider voluntary CORE Certification to publicly communicate their systems meet the CAQH CORE Rayment & Remittance Operating Rule requirements.
Keeping Up with the CORE-required Maximum Enrollment Data Sets
If you are tasked with implementing the EFT & ERA Enrollment Data Rules mandated under HIPAA, you will find the necessary information here to comply with these operating rules.
Background
The CAQH CORE Payment & Remittance Operating Rules support the healthcare industry's transition to electronic payment and remittance advice.
Two of the five CAQH CORE Payment & Remittance Operating Rules address the barriers to greater provider EFT and/or ERA enrollment. The EFT & ERA Enrollment Data Rules outline maximum sets of standard data elements to be collected by a health plan or its agent during provider enrollment in EFT and/or ERA. The rules also outline a flow and format for collection of the data elements, among other requirements.
The EFT & ERA Enrollment Data Rules also recognize the need for ongoing maintenance of the CORE-required Maximum EFT & ERA Enrollment Data Sets and establishes a policy and process to review the Enrollment Data Sets no less than annually. From 2014 - 2022, review of the Enrollment Data Sets was conducted annually, with limited in-scope submissions from the industry and no substantive adjustments to the data sets.
