Better data.
Fewer burdens.
Drawing on professional and practice information already entered and verified by providers, the CAQH Provider Data Portal improves health plan directories while reducing redundant, inefficient processes.
Improve Directory
Accuracy and Compliance
To enhance accuracy, CAQH's provider directory management solution applies advanced analytics to data entered, updated and confirmed by physician practices. This multi–layered approach improves data quality, reduces the burden on providers and supports state and federal regulatory compliance.
For delegated groups, administrators are able to centrally manage non-sensitive directory information and make changes to locations, phone numbers and other information once and push it to all providers.
A Streamlined Approach for Providers, Payers and Groups
Providers
Physician practices receive fewer outreach calls from plans and are more accurately reflected in member directories.
Health Plans
Health plans obtain more accurate data and achieve greater regulatory compliance with less provider abrasion.
Provider Groups
Group administrators can manage directory data in one place and have changes apply to all providers.
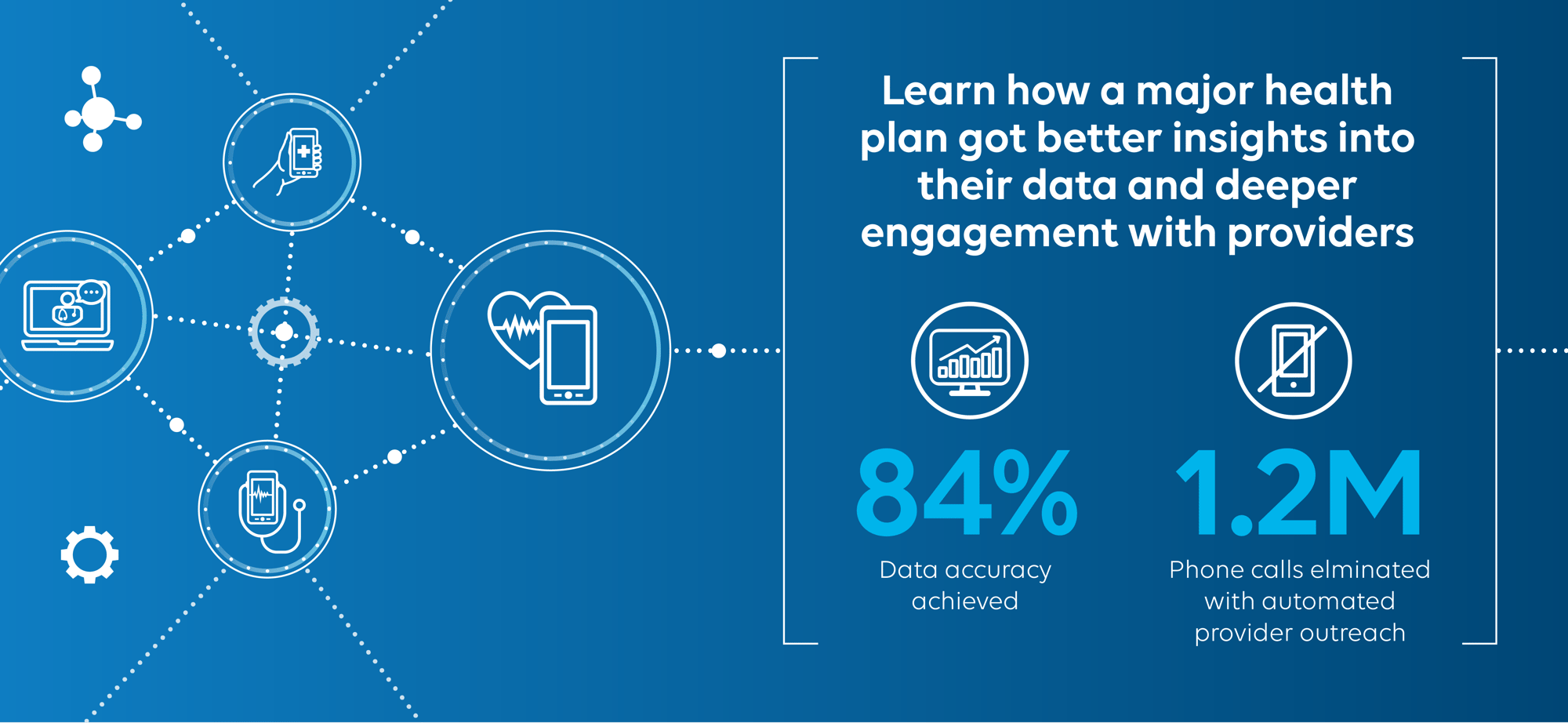
A National Health Plan Achieves 84% Directory Accuracy
One of the nation's largest payers struggling with directory accuracy turned to CAQH for an efficient way to improve data quality without placing additional burdens on providers in its network.
CAQH Directory Management at a Glance
Confirmed provider profiles in CAQH's directory management solution
Providers who have confirmed their data within the past 120 days
Health plans participating in CAQH's directory management solution
Help members find the
provider that is right for them
Provider and Practice Details
CAQH collects information on health equity, race, ethnicity, language and other factors to help members find the provider that is right for them.
Telehealth Availability
The provider directory management solution includes information on telehealth services offered by providers, including the type of service and platform used.
Network Adequacy
Plans can access detailed data to assess, understand and manage provider networks.
“We have found that the quality of data received via the directory management solution is higher than any other attestation channel we have today.”
One of the nation's largest health plans
"My account manager delivered on-the-spot, thorough guidance to answer my question and even followed up with helpful resources."
Health plan serving communities in Massachusetts
"My account manager had an understanding of our unique needs and was able to translate that insight to support our directory management and credentialing initiatives."
Mid-size health plan in the Midwest
Provider Directory Management
Improve data accuracy while saving time and money by reducing efforts to collect and verify information. Learn more about our Directory solution today.

.png)